Why do some knee replacements get stiff?
Orthopedic Patient Updates
written by Dr. Will Kurtz
Why do some knee replacements struggle to get their motion while others easily obtain great motion?
This article attempts to explain why some patients achieve full range of motion after a knee replacement and why others struggle. Obtaining just the correct amount of stability without instability requires a patient specific approach.
Stiffness vs. Unstable
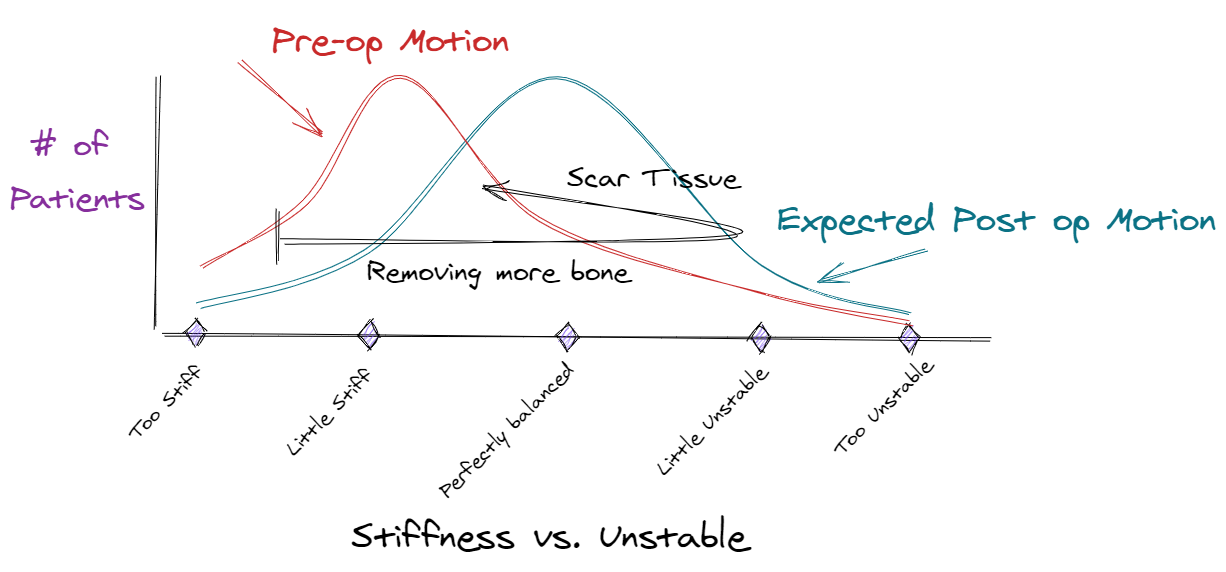
Stiffness and instability are two opposite sides of the same spectrum. There is a bell shaped distribution curve that describes the number of normal patients with a stiff knee, a normally balanced knee, and an unstable knee. As patients develop arthritis and becomes less active in their later years, the distribution curve stiffs to the left with less range of motion than a normal, non-arthritic knee. This stiffness might be a flexion contracture (not getting the knee fully straight) or limited flexion (not being able to bend the knee all the way back).
Fig. 1 - Distribution of Stiff vs. Unstable Knees - Normal vs. Arthritic
Amount of bone resection during surgery affects stiffness
During surgery, any surgeon can remove more bone, release more soft tissue, and/or use thinner implants to give the knee replacement more motion. Surgeons call this “putting the knee in loose”, but this increases the possibility of post-operative knee instability in some patients (Fig. 2). Putting the knee in loose effectively shifts the distribution curve to the right and is beneficial for patients with pre-operative stiffness. If a patient is stiff before surgery, the surgeon will remove more bone during surgery which can improve post-operative range of motion.
Any surgeon can remove less bone, release less soft tissue, and/or use thicker implants to give the knee replacement more stability. Surgeons call this “putting the knee in tight”, but this increases the possibility of post-operative knee stiffness in some patients. Putting the knee in tight effectively shifts the distribution curve to the left and is beneficial for patients with pre-operative instability.
Fig. 2 - Putting the Knee in Loose
Scar Tissue affects Stiffness
Some patients will significantly swell and make considerable scar tissue in the first couple of months after their knee replacement surgery. The more scar tissue a patient makes, the stiffer their knee will likely become. (Fig. 3) Scar tissue effectively shifts the curve to the left. When surgeons expects a patient to make extensive scar tissue, the surgeon will remove more bone during surgery. Patients with diabetes, a history of stiffness/swelling after surgery, and limited pre-operative motion are known to make extensive scar tissue.
Fig. 3 - Scar Tissue increases Stiffness
Physical Therapy affects Stiffness
All surgeons expect their patients to have some post operative swelling and some scar tissue formation. The patients perform physical therapy to combat the effects of the scar tissue formation.(Fig.4) If a patient makes more scar tissue than expected and struggles to regain their range of motion, then the patient will likely do more physical therapy and/or consider a manipulation (the patient receives anesthesia, and then the surgeon gently flexes the knee to the maximum amount).
Fig. 4 - Physical Therapy decreases Stiffness
Swelling and Range of Motion
In general, most surgeons make their knee replacements feel “balanced” on the operating table with the expectation that the way the knee feels on the operating table will approximate the way the knee will feels when the patient is fully recovered in 2-3 months. Surgeons typically expect most patients to swell and lose some of their initial motion during the first few weeks after surgery. As the swelling subsides and physical therapists work on range of motion, the patient should regain their full range of motion. Their knee replacement should feel like it did on the operating table.(Fig.5) In an unpublished study that I did involving 300 of my knee replacements, the patients who had greater than 2 cm of swelling on post op day #2 ended up with 12 degrees less flexion than the patients who had less than 2 cm of swelling. Excessive swelling can have a deleterious effect on knee range of motion.
Fig. 5 - Swelling vs. Range of Motion
Considerations for how to perform knee replacement
How loose or tight to initially make a knee replacement is constantly debated among surgeons and depends on many factors:
How stiff is the patient’s knee before surgery?
How much scar tissue does the surgeon expect the patient to make?
How hard will the patient work at physical therapy?
What is a perfectly balanced knee replacement supposed to feel like in the operating room?
Which complication is the surgeon more interested in avoiding; instability or stiffness?
It is important to realize that any surgeon could make all of their knee replacement patients easily obtain normal range of motion by removing extra bone, but then a number of these patients would have problems with knee instability. Any surgeon could make all of their knee replacement patients have great stability by removing less bone, but then a number of these patients would have problems with their knee range of motion. Therefore, most patients should expect to initially be stiff for a few months after surgery and approach an ideal balance between stability and range of motion when their knee is healed and the swelling has left (i.e. 3-6 months).
A patient should not get discouraged if they have to work a little harder at achieving their range of motion. Likewise, a patient should not be overly excited if they easily obtain early range of motion.
How Surgeons assess Stability during Surgery
This stability of the knee replacement (how tight or loose) in the operating room is a subjective feel. Many surgeons make provisional bone cuts and insert spacer blocks that represent the thickness of the knee replacement. The surgeon applies a side to side force to the knee and observes how much the knee opens up on one side or the other. If the knee does not open up like the surgeon wants, then the surgeon either removes more bone, releases more soft tissue, or uses a smaller implant.
Surgical navigation (and robotics) can also provide some objective data to intra-operative stability. The navigation arrays are drilled into the femur and tibia. The surfaces of the knee joint is registered. The surgeon can then measure the flexion and extension gaps while the surgeon applies a force from side to side.
Risk Factors for Stiffness
Patient factors that increase the risk of post operative stiffness are:
Limited pre-op motion
Previous knee surgeries
Previous history of stiffness after other joint surgeries.
Ankylosing Spondylitis
Patella Baja
Likely diabetes
Likely obesity
There are some surgical risk factors that increase the risk of post operative knee stiffness.
Improper balancing between the flexion and extension gaps
Oversizing the components
Joint line elevation
Inadequate bone resection
Posterior Stabilized (PS) implants typically achieve more flexion than Cruciate Retaining (CR) implants, but also have more instability issues.
How do you limit post operative Stiffness?
Patients should follow their surgeon’s instructions. For me, that means patients initially concentrate on range of motion above all else. When patients walk too much or stand too long, they tend to increase their bone stress pain, increase their swelling, and lose range of motion. This over-activity can set a patient back. For that reason, I encourage patients during the first 2-3 weeks to walk infrequently for short distances like from one room to the other. Patients should avoid walking outside for exercise for the first 5-6 weeks. Patients should also:
Elevate their leg.
Ice their leg every few hours.
Take anti-inflammatory meds as tolerates.
Do hourly heel slides.
Keep the knee straight when possible. Put a pillow only under the operative ankle, so the operative knee is slightly elevated off the bed. Never put the pillow under the knee as this keeps the knee slightly bent and leads to a flexion contracture.
Steroids in some situations.